Population health management can't just focus on physical health - providers must also take responsibility for a broader range behavioral health concerns to succeed in a changing environment.
 There is an odd division in the healthcare world that creates an
unfortunate schism between the clinical care of a patient and his mental
and behavioral wellbeing.
There is an odd division in the healthcare world that creates an
unfortunate schism between the clinical care of a patient and his mental
and behavioral wellbeing.
Even as population health management programs grow and expand,
forging new bonds between healthcare organizations and community
services that help patients cope with socioeconomic shortfalls, medicine
still largely operates with its blinders on.
The historical precedent for this attitude is a long and strong one.
Traditionally, physicians focused on physical wellness, diagnosing and
treating ailments of flesh and bone. Psychologists, psychiatrists,
social workers, and councilors operated in a completely separate sphere,
with only a tenuous link between the two.
Only a few short decades ago, skepticism over the relationship
between physical and mental health was so widespread that Dr. Brock
Chisholm, the first Director-General of the World Health Organization
(WHO), was considered revolutionary and radical
for stating that mental healthcare is inseparable from physical
wellbeing, while stressing the importance of treating the whole patient
for optimal outcomes.
To the credit of forward-thinking professionals, rule makers, and advocates from across the care continuum, the integration of mental and physical healthcare has advanced rapidly since then.
Under continuously evolving guidelines
for care quality improvement, primary care providers (PCPs) are
encouraged to perform basic screenings for depression, substance abuse,
and interpersonal violence. PCPs can prescribe appropriate medications
and make referrals to mental healthcare specialists.
Assessing the mental healthcare landscape
Despite these ongoing efforts, the primary care ecosystem faces
several major challenges when it comes to assessing high-risk mental
health patients and ensuring that they can access effective,
cost-conscious services.
First of all, many of the neediest mental health patients don’t have a
relationship with a PCP, the Agency for Healthcare Research and Quality
(AHRQ) points out.
Patients with psychotic disorders are 45 percent less likely than other
patients to have an established primary care provider, while patients
with bipolar disorder are 26 percent likely to have a relationship with a
PCP.
Even those patients who do have a PCP relationship may not receive a
diagnosis from their primary care clinicians. In 2012, Professor
Michael Porter from the Harvard Business School estimated
that PCPs only recognize and identify half of all mental illnesses in
their patients. And only half of those patients with a recognized
disorder are offered medication to treat their condition.
Barriers to care access, including cost, distance, and ability make
mental health patients up to seven times less likely than other patients
to receive proper treatment from any providers at all. AHRQ identified
mental health disorders as the most costly condition in 2006, topping
more prominent acute and chronic diseases like cancer, heart disease,
asthma, and trauma-related conditions.
Four percent of young adults put off mental health treatment due to
high costs, the report states. Before the Affordable Care Act instituted parity
between medical and mental healthcare coverage, nearly 20 percent of
Americans had no insurance coverage for mental healthcare.
Out-of-pocket expenses for mental healthcare services were higher than
any other type of treatment for adults and children alike.
From a population health management perspective, these grim
circumstances get even more complicated. Patients with chronic diseases
such as diabetes, Parkinson’s and Alzheimer’s, and cardiovascular
disease, as well as those living with cancer, experience high rates of
depression, the CDC says.
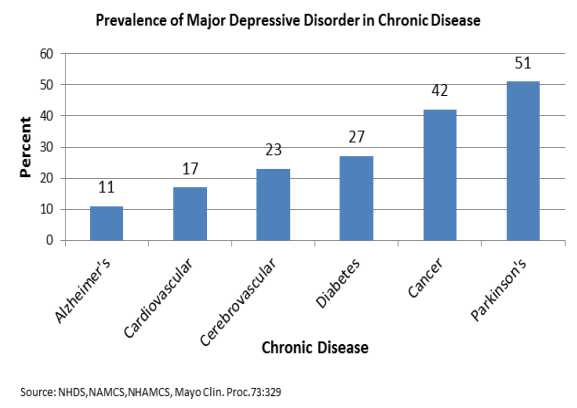
More than half of patients with Parkinson’s also experience major
depressive disorder, while 42 percent of cancer patients, 27 percent of
diabetics, and 17 percent of cardiovascular disease patients also cope
with depression. A 2014 study found that feelings of extreme loneliness
and isolation in seniors increased their risk of premature death by an unsettling 14 percent.
In addition to being a major cause of disability and lost quality of
life, depression and other concurrent mental health disorders can make
appropriate chronic disease management extremely difficult for
patients.
Just 30 percent of patients
with mental illness are even screened for chronic diseases like
diabetes, a recent study found. And the odds of a patient with
depression being non-adherent to his or her medications are 1.76 times greater than patients without depression, a 2011 study found.
For healthcare providers who are starting to invest in value-based
reimbursement programs, accountable care organizations, or other
contracting frameworks that pin payments to outcomes, these statistics
should be extremely alarming.
If providers acknowledge the fundamental tenant that mental and
physical healthcare are inextricably linked, they must therefore improve
the delivery of mental healthcare to succeed in quality-based payment
programs and population health management initiatives..
What is standing in the way of better mental healthcare?
As one might expect, however, finances are a major barrier in
addition to being an incentive. Payers who are eager to support
value-based reimbursement as a way to reduce provider-sided spending are
also pushing higher deductibles and copays onto patients in an effort
to encourage smarter decision-making.
This can produce unintended and counterproductive consequences for
patients with significant chronic disease management needs or long-term
medications that require hefty investments each month, warns a study newly published in the American Journal of Managed Care (AJMC).
“Increases in what patients have to pay have resulted in the early
mismanagement of some diseases, potentially leading to increased need
for acute care, emergency department (ED) care, and long-term care,”
explain researchers from the University of Arkansas. “For example, lack
of adherence to diabetic medicine, due to reluctance of the patient to
pay, can lead to medical complications and an overall increase in cost
to the healthcare system.”
Almost 45 percent of patients who visit the emergency department, a
traditionally expensive option that many new population health
management programs discourage, suffer from a mental illness and/or a
substance abuse issue, the study states. Mental health disorders are
also responsible for up to ten percent of pediatric hospitalizations.
With up to $4 billion in yearly spending dedicated to the treatment
of mood disorders like bipolar disorders and depression, value-based
reimbursement and population health management programs have a massive
opportunity for slashing costs – but they must do so in a sensitive and
patient-appropriate way.
The researchers suggest that “there may be value in reducing patient
copays and deductibles in the management and screening of some
diseases,” including mental health conditions.
“Establishing price responsiveness for the treatment and management
of various diseases, then applying the most effective pricing for
deductible and co-pays, is imperative to optimize the outcome and proper
application of any [value-based reimbursement] program.”
Technology deficiencies are also a major culprit in the gulf that
remains between medical and mental health. As a result of being
considered a separate entity for so long, many behavioral health
organizations exist a world apart from the EHR ecosystems and health
information exchange networks growing among ambulatory and inpatient
care providers.
Behavioral health organizations have been largely ineligible for the
EHR Incentive Program dollars that sparked a rush of technology adoption
among other providers, leaving them out of the health IT loop.
Legislation that hoped to provide
incentive payments to mental healthcare providers stalled in the House
of Representatives in the summer of 2015, dashing hopes that behavioral
health organizations could collect the tail end of meaningful use
dollars.
While those behavioral health providers who have adopted EHRs are generally satisfied
with their decision, integrating their data into the primary care
system has been no easy task. In addition to the widespread problems of data siloes and differing standards that prevent EHRs from communicating effectively, mental health data faces its own particular privacy and security concerns.
How can healthcare providers make positive patient care changes?
Adjustments to value-based reimbursement structures may be in the
hands of payers, who are still feeling their way through the shift from
fee-for-service payments, but providers can take several proactive steps
of their own to improve the integration and delivery of mental health
services.
The first task is to commit to becoming a patient’s central resource
for all types of care. Providers participating in the patient-centered
medical home (PCMH) model and many accountable care organization
arrangements have already started to adjust to this hub-and-spoke
mentality of care delivery, and some integrated delivery models have
even made it a point to place the offices of behavioral health services
right down the hall from their PCPs.
Primary care providers can also leverage their investments in health
IT tools to expand their patients’ ability to discuss their mental
health concerns in a secure, private, low-cost, low-effort manner. Patient portals may be a promising avenue for improving communication, a separate AJMC article recently found.
Patients were eager to conduct e-visits with clinicians about mental
health topics, even when the online tool did not specifically promote
mental health as one of the primary complaints providers could address.
Combined with evidence from another new study
that found higher rates of online patient engagement for consumers
facing large out-of-pocket costs for basic care, it is apparent that the
use of patient portals, secure emails, and other health IT
communication methods is popular among patients, and may increase the
likelihood of diagnoses and treatment for behavioral health conditions
with little added cost on either side of the equation.
Healthcare organizations can also take advantage of existing community services
that help patients address and overcome socioeconomic challenges, such
as food and housing insecurity, lack of transportation, and educational
needs, which can negatively impact chronic disease management and
consistent contact with the healthcare system.
A 2014 study from JAMA Internal Medicine
found that economic insecurity was directly linked with poor chronic
disease control. With the majority of patients in the study
experiencing at least one major economic hardship, more than a quarter
said they were non-adherent to their medications, while 46 percent were
unable to control their diabetes appropriately.
As the federal government works to improve awareness
around the links between mental health, socioeconomic hardship, and
physical wellbeing, primary care providers can take advantage of grants
and other funding opportunities that attempt to foster meaningful
partnerships across the care continuum.
“We recognize that keeping people healthy
is about more than what happens inside a doctor’s office, and that’s
why, for the first time, we are testing whether screening patients for
health-related social needs and connecting them to local community
resources like housing and transportation to the doctor will ultimately
improve their health and reduce the cost to taxpayers,” said HHS
Secretary Sylvia M. Burwell during a recent announcement for $157 million in funding to strengthen provider bonds with their communities.
Holistic population health management is among CMS’ top quality improvement goals for the next few years, the agency said
in January of 2015. As value-based reimbursements and other patient
care coordination and cost reduction strategies place a greater emphasis
on cooperation and communication across an expanded care continuum, the
ability of the healthcare system to integrate mental and clinical
healthcare will directly impact their financial success.
Healthcare providers can start to drive innovations and improvements
in this challenging but critical important area by taking the lead in
building relationships with their partners in behavioral health and
community services to develop a robust, effective, and patient-
centered strategy for the entire spectrum of a patient’s healthcare needs.
Learn How to generate 6 Million visitors, 100,000 Leads and $144,595 profit online
ReplyDeleteTry it nearly FREE: $1.00 for an entire month! See for yourself that it works. Then, continue for just $97 per month. Cancel any time. 60 day money back guarantee. Even a short membership could send you AUTOPILOT leads and commissions LONG after you're gone if for some reason you had to cancel.
http://www.moneymakerstore.com/2016/01/a-way-to-generate-6-million-visitors.html