Under a new ruling issued by federal government agencies, health payers may be able to reimburse emergency care providers whatever fee deemed applicable.
 As the year is coming to a close and many are getting ready to
celebrate the holidays, it is important to look toward the coming year
and prepare for healthcare insurance trends expected to impact the
market. Over the last several years, both the Patient Protection and
Affordable Care Act along with the Health Information Technology for
Economic and Clinical Health (HITECH) have made significant changes for
the healthcare industry.
As the year is coming to a close and many are getting ready to
celebrate the holidays, it is important to look toward the coming year
and prepare for healthcare insurance trends expected to impact the
market. Over the last several years, both the Patient Protection and
Affordable Care Act along with the Health Information Technology for
Economic and Clinical Health (HITECH) have made significant changes for
the healthcare industry.
It’s important to understand how various health reform initiatives
will continue impacting the health payer market. Below we outline four
healthcare insurance trends that payers should watch out for in 2016.
ACOs will consolidate and continue to bring cost savings
Today, Accountable Care Organizations (ACOs) are becoming a real
stronghold throughout the healthcare industry, as these partnerships are
bringing more providers as well as payers to discuss and plan ways to
garner cost savings.
In an interview,
Ted Schwab, Managing Director at Huron Healthcare, stated, “What folks
have overlooked is that the ACO movement has been an organizing force
throughout the healthcare industry and it’s got hospitals and doctors
for once under the same umbrella talking about efficiencies, clinical
protocols, and ways to save costs.”
“There are now north of 700 of these organizations in the United
States of America,” Schwab explained. “If you think about where the
industry has been for the last 100 years, it’s been a mom-and-pop
fragmented industry. Now you have 700 organizations with folks at least
talking to each other. It’s going to take a while. We’re at the very
beginning of this movement and I could not be any more encouraged.”
“I think that both the Medicare Shared Savings Program and the ACO
industry will evolve. We will see a massive consolidation of ACOs just
like we’re seeing consolidation in the rest of the healthcare industry
so folks can get to scale and use that scale to leverage efficiencies.”
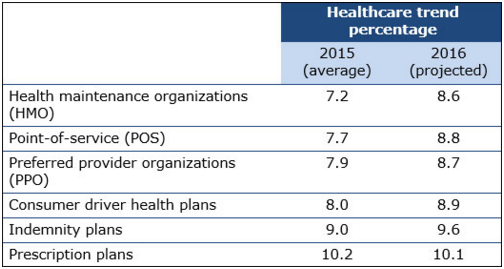
Healthcare premiums expected to rise
When it comes to claims reporting and medical billing, health
insurers are reporting that premiums will rise above regular inflation
rate in 2016, according to the Spring Healthcare Trend Survey from Wells Fargo Insurance. Out of all healthcare insurance trends, this is an important one to watch out for.
The reason for the increase in healthcare premiums many are reporting
is due to predictions that medical claim costs will rise by 7 to 10
percent next year. Additionally, rising costs in drug prices are also
leading to bigger premiums for employers and consumers, the survey
found. Healthcare claims trends are also expected to rise for the
majority of products in 2016.
Emergency care reimbursement will lack restrictions
Under a new ruling issued by federal government agencies, health
payers may be able to reimburse emergency care providers whatever fee
deemed applicable. The Department of the Treasury, the Department of
Labor and the Department of Health and Human Services issued a final ruling that states insurers can pay physicians working in emergency rooms “whatever they like,” according to a press release from the American College of Emergency Physicians (ACEP).
Emergency care providers are likely to be against this type of
legislation especially since they have provided adequate feedback to the
Centers for Medicare & Medicaid Services over the years. ACEP is
currently considering taking legal action against this new ruling, as it
would heavily favor health payers ahead of emergency care providers and
the patient community.
The ruling establishes that within states that have prohibited
balance billing, minimum payment standards will not be required. Balance
billing is essentially a practice in which health plans pay a very low
reimbursement rate and physicians bill patients for the unpaid balance.
Research shows that many patients today are foregoing obtaining
medical care until it becomes a complete emergency because of high
deductibles or out-of-pocket expenses. This is a significant problem and
legislation that allows payers to cover whatever costs they deem
necessary would only exacerbate the issue. When it comes to healthcare
insurance trends, this one is likely to negatively impact emergency care
providers in the coming year.
“This new ruling will significantly benefit health insurance
companies at the expense of physicians, because they know hospital
emergency departments have a federal mandate to care for everyone,
regardless of ability to pay,” Dr. Jay Kaplan, President of ACEP, said
in a public statement.
“They will continue to shift costs onto patients and medical
providers, as well as shrink the number of doctors available in
plans. Instead of requiring health plans to pay fairly, this ruling
guarantees that insurance companies can pay whatever they want for
emergency care.”
Bundled payments and value-based care gain popularity
Today, healthcare providers are already moving away from the standard
fee-for-service payment model and adopting alternative reimbursement
strategies. The Medicare Access and CHIP Reauthorization Act of 2015
(MACRA) was passed earlier this year and it will also push forward the
advancement of value-based care.
MACRA brings forward more focus on alternative payment models a
nd
performance quality measures, which means payers will begin to
reimburse providers for quality healthcare services instead of merely
the quantity of services provided, as seen with the fee-for-service
payment system.
Additionally, the Centers for Medicare & Medicaid Services (CMS)
are attempting to spread bundled payments throughout various aspects of
the healthcare industry, particularly among joint replacement surgeries.
In an interview with HealthPayerIntelligence.com,
Jeremy Earl, Associate at McDermott Will & Emory, clarified, “From
my perspective, I’m a big believer in the shift away from
fee-for-service payments. Today, you get a critical mass of providers
who are being compensated on whether the care they provide is
cost-effective and high-quality versus just providing more care.”
“The bundled payment demonstration project on a voluntary basis has
been extremely popular with a lot of providers and now they’re rolling
it out to be mandatory. That’s just one example of the program put in
place by the Affordable Care Act transforming how providers are paid.”
No comments :
Post a Comment